|
|
|
|
|
|
#10-16 Connexion Farrer Park
Medical Centre
1 Farrer Park Station Road
Singapore 217562
[getting there]
|
|
|
|
|
|
| Phone : | +65 67330846 | | Fax : | +65 67330849 | 24Hr Answering
Service : | +65 65358833 |
|
|
|
|
|
|
| Mon - Fri : | 9:00am - 5:00pm | | Sat : | 9:00am - 1:00pm |
|
|
|
|
|
|
|
Obesity Surgery (Bariatric Surgery)
|
Obesity: a global epidemic
The World Health Organization estimates that globally, there are more than 1 billion overweight adults with at least 300 million of them obese. In the US, two out of every three adults are overweight and one in three are obese. This trend in obesity is global and Asian countries have not been spared: recent figures show that in Singapore, 34% of adults are overweight and 14% are obese.
|
Why are we seeing an increasing prevalence in obesity? There are many factors involved: on the one hand, there is a global shift in diet towards processed and fast foods – these are energy-dense diets which are high in fat and sugar, but low in vitamins, minerals and micronutrients. At the same time, we all lead increasingly sedentary lives – in almost every field of work, we now have machines to perform tasks which generations ago were done by hand.
|
How do we define obesity?
Overweight and obesity are commonly assessed using body mass index (BMI). Your BMI is calculated as follows:
BMI = Weight (in kg) / Height * Height (in m)
|
|
| < 18.5 | Underweight | < 18.5 | | 18.5 – 24.9 | Normal | 18.5 – 22.4 | | 25.0 – 29.9 | Overweight | 22.5 – 27.4 | | 30.0 – 34.9 | Obese | 27.5 – 32.4 | | 35.0 – 39.9 | Severe obesity | 32.5 – 37.4 | | >40.0 | Morbid obesity | >37.5 |
|
The lower BMI ranges for overweight and obesity in Asians are based on the fact that Asians have a higher risk for Type 2 diabetes and cardiovascular disease at a lower BMI. In addition Asians generally have a higher percentage of body fat than white people of similar age, sex and BMI [see reference 1].
|
How does excess body fat & obesity impact health?
Obesity has been shown in many large, long-term epidemiologic studies to be associated with increased mortality (risk of death) [see reference 2]. In younger people with severe obesity, life expectancy is reduced by an estimated 5 to 20 years [see reference 3].
|
|
Obesity is associated with adverse metabolic effects on blood pressure, cholesterol, triglycerides and insulin resistance. The risk of developing Type 2 diabetes and hypertension rises steeply with increasing body fat: approximately 90% of Type 2 diabetics are either overweight or obese.
|
|
Obesity is also associated with a host of medical conditions including cardiovascular diseases, respiratory difficulties, chronic degenerative joint diseases and musculoskeletal problems, gallbladder disease and skin problems. There is also an increased risk of developing cancer of the breast, colon, prostate, endometrium, kidney and gallbladder.
|
In other words, obesity decreases life expectancy and is associated with multiple medical problems (including diabetes, hypertension, cardiovascular disease and cancer) all of which contribute towards a poorer quality of life.
|
Rationale for surgery: why perform an invasive surgical procedure for obesity?
We need to stop thinking of obesity as a merely cosmetic problem: it is a health hazard. Obesity is a chronic disease with serious implications on the health of an individual: it reduces life expectancy, decreases quality of life and is associated with complications from multiple medical conditions including hypertension, Type 2 diabetes, cardiovascular and respiratory diseases. It also increases the risk of developing several forms of cancer.
|
|
It follows then, that the treatment goal in obese individuals should be an improvement in health achieved through significant and sustained weight loss that reduces life-threatening risk factors, improves performance of activities of daily living and improves quality of life.
|
|
Published scientific reports document that non-operative treatment methods have not been effective in achieving significant and sustained weight loss in severely obese individuals [see reference 4]. Non-operative weight reduction programmes incorporating long-term drug therapy (at least one year on medication) are not effective: typically one third of patients drop out from these programs and average weight loss even after long term medication is < 5kg [see reference 5]. Any weight loss is often regained over time as millions of ‘yo-yo’ dieters will attest.
|
|
Surgical treatment is medically necessary because it is the only proven method for long-term, sustainable weight control in the severely obese. Surgery for obesity (bariatric surgery) is not a cosmetic procedure: it does not involve removal of excess fat by suction or excision. Instead, bariatric surgery is surgical manipulation of the gastrointestinal tract in such a way that food intake is restricted; some bariatric surgical procedures are also designed to alter the absorption of nutrients.
|
|
Published data show that surgical treatment of obesity is
|
What are the indications for weight reduction surgery?
Weight reduction surgery is indicated in individuals with:
|
- severe obesity WITH obesity-related comorbidities [obesity related comorbidities’ refer to health problems arising as a result of obesity. These include hypertension, Type 2 diabetes, hyperlipidaemia, sleep apnoea, osteoarthritis amongst others]
- morbid obesity (regardless of whether or not comorbidities are present)
|
Please see table above for definitions of severe and morbid obesity in Caucasians and Asians.
|
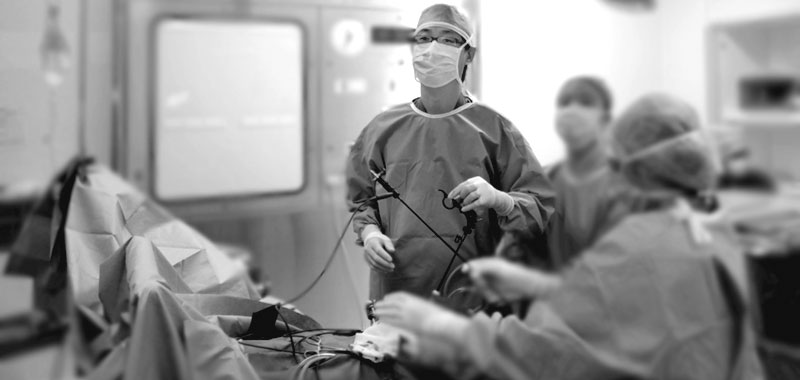
Weight Reduction (Bariatric Surgery) for Obesity
Weight reduction surgery is mostly performed using minimally invasive (keyhole) techniques. The following are some of the more commonly performed bariatric procedures:
|
| • Laparoscopic Adjustable Gastric Banding | | This procedure involves placing an inflatable silicone band around the upper portion of the stomach. The band creates a small gastric pouch and restricts the amount of food consumed; it also induces early satiety even after consuming small amounts of food. The inflatable band is connected by tubing to a ‘port’ which is implanted under the skin. This constricting, inflatable band may be tightened by injecting saline into the port, allowing the surgeon to assist in regulating food intake. | 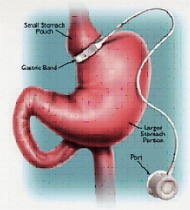
[See Larger] |
|
| • Laparoscopic Sleeve Gastrectomy | | This procedure aims to restrict food intake by decreasing the size of the gastric reservoir. Using specially designed surgical staples, the left side of the stomach is removed, leaving a narrow gastric tube. Unlike the gastric band, this operation does not involve implanting an artificial device into the abdomen. | 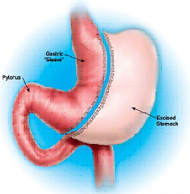
[See Larger] |
|
| • Laparoscopic Roux-en-Y Gastric Bypass | | This procedure involves the creation of a small gastric pouch using surgical stapling devices. The small intestine distal to the duodenum is divided (again with staplers) and a limb of intestine (the Roux limb) is then joined to the small gastric pouch. As one can see from this diagram, the food stream ‘bypasses’ most of the stomach, hence the term gastric bypass. | 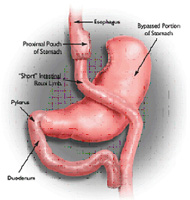
[See Larger] |
|
Each of these surgical procedures has its own advantages and disadvantages. The relative merits of these operations will not be discussed here. Our surgeon will be able to recommend a particular procedure only after a detailed and thorough assessment of each patient.
|
|